Keyhole Disc Surgery(PELD)
DISC PROLAPSE
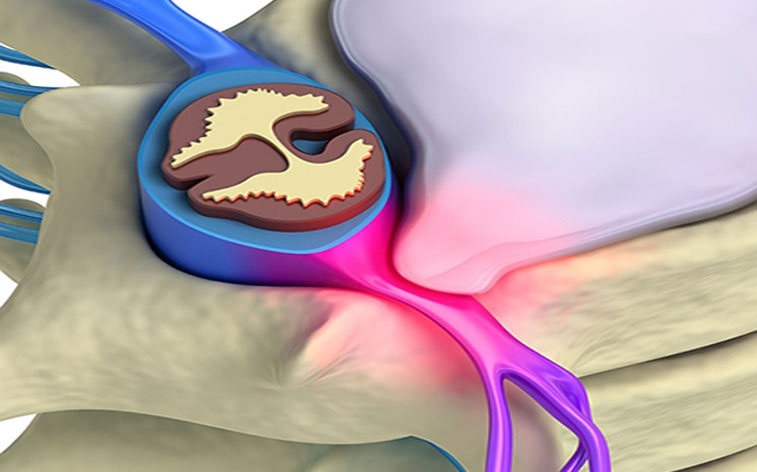
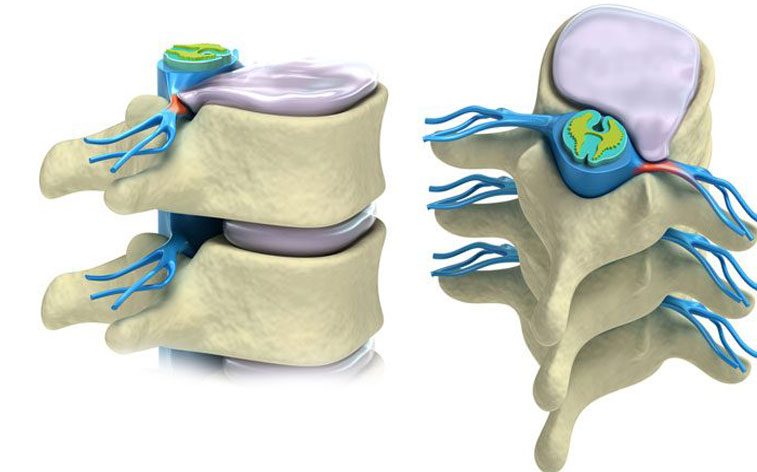
What is disc prolapse?
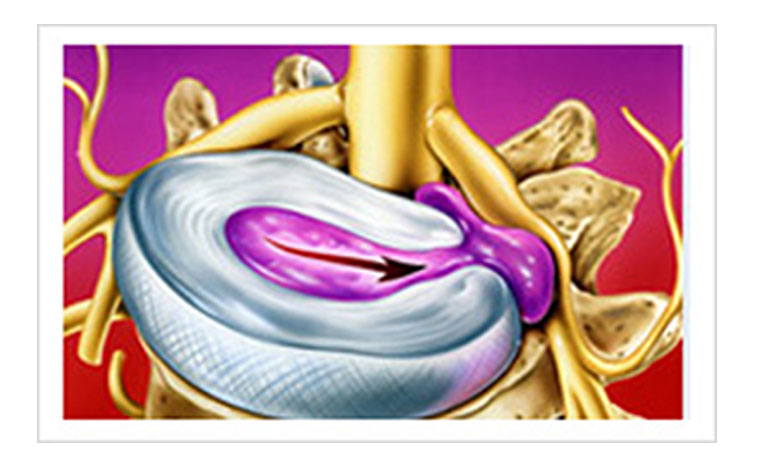
Disc prolapse is a condition in which the intervertebral disc slips from its normal position. This slip can occur when the patient tries to lift a heavy weight and experiences a catch in the back. This slip can also occur after a heavy exertion, prolonged travel or unaccustomed activity or fall. Sometimes, disc prolapse can occur without any reason.
Symptoms of disc prolapse
- Back pain: Back pain may start on its own or after lifting heavy weights. Pain increases on coughing or straining. Sometimes, pain may be severe and there may be difficulty in sitting, standing and walking.
- Leg pain or sciatica: If the disc prolapse is pressing on the nerves, patient will get shooting pain in one or both the legs called sciatica.
- Patient may experience numbness or weakness of one or both the legs.
- Rarely, there may be difficulty in passing urine or motion. It is an emergency because if surgery is not done within 48 hours, patient will not recover for the rest of the life.
Diagnosis of disc prolapse
Disc prolapse can be diagnosed by clinical examination. When the leg is lifted straight up, if there is pain in the leg, it is suggestive of disc prolapse (straight leg raising test). By examining the muscle power, sensations and reflexes, doctor is able to diagnose the level of disc prolapse. The diagnosis is confirmed with x ray and MRI scans.
Treatment of disc prolapse
90 percent of disc prolapse can be cured without any surgery. Non surgical treatment includes rest, painkillers, belt, traction, exercises and physiotherapy. However, in 10 percent of cases, surgery is required.
Types of surgery for disc prolapse
Previously, open surgery (Laminectomy and discectomy) was performed for disc prolapse. However, laminectomy is a destabilizing surgery. Patient needs to stay in the hospital for two weeks and needs to take rest at home for three months. The back and its supporting structures are permanently scarred. The patients continue to have back pain and are disabled for the rest of the life. There are long term complications such as spinal instability, epidural fibrosis, and recurrent disc prolapse. If there is any complication, it will ultimately require spinal fusion. With the advent of microdiscectomy, these complications are less but significant drawbacks of open surgery still remain. THE LATEST SURGERY FOR DISC PROLAPSE IS CALLED ENDOSCOPIC DISC SURGERY WHICH IS A KEY HOLE SURGERY..
TRANSFORAMINAL STEROID INJECTION (TFSI)
Previously, epidural steroid injection was used as a treatment modality for disc prolapse. The problem with traditional epidural steroid injection is that it is given in the epidural space randomly and not at the site of pathology, i.e. inflamed nerve root. Hence traditional epidural steroid injection does not give good results. In transforaminal steroid injection, the affected nerve is located under image guidance and steroid is injected into the site of pathology, i.e. around the inflamed nerve root. It is again a day care procedure and the results are very good. It is also used when there is doubt about the cause of pain. If the pain is discogenic, it will relieve with TFSI. If the pain recurs after sometime, patient will have good results with endoscopic disc surgery.
KEY HOLE DISC SURGERY
The development of transforaminal endoscopic procedures is the answer for all problems of open surgery. Now it is possible to remove a herniated disc with a 7mm incision under local anaesthesia. It is a day care procedure with no hospital stay. Patient can come in the morning for the surgery and go home in the evening. The advantages of percutaneous endoscopic discectomy are
- Minimally invasive
- Least morbidity
- Done under local anaesthesia
- No blood loss
- No IV fluids
- No epidural fibrosis
- Day care procedure
- Reduced rate of recurrence
- Cost effective
- Rapid recovery

This surgery does not burn any bridges for future. Even if the patient is unfit for open surgery, endoscopic surgery can be performed without any risk. We can guarantee 90-95% excellent results with percutaneous endoscopic disc surgery. Even if open surgery is required in the future, it can easily be done because there is no fibrosis. We have not faced any major complications with this new procedure.

PRE OPERATIVE CHECKLIST
Patient needs to be on empty stomach for at least six hours before the surgery. If the patient has diabetes or hypertension, it should be under reasonable control. If the patient is on anticoagulants such as aspirin or clopidogrel, they can be continued. If your antihypertensive has to be taken few hours before surgery, it can be taken with sips of water. Patient needs to undergo blood tests and ECG as advised by the doctor and this will take about one hour. Even if the patient is unfit to undergo surgery under general or spinal anaesthesia, keyhole disc surgery can be done because it requires only local anaesthesia and sedation.
WHAT IS DONE DURING SURGERY
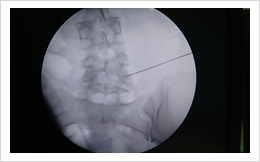
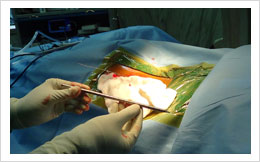
Surgery is done under local anaesthesia, in prone position. Skin is prepared with antiseptic solutions and draped to isolate the operative field. Skin is anaesthetised with local anaesthesia. Anaesthetist will a dose of sedative and analgesics to make you comfortable. An 18 gauge needle is inserted into the disc space under image control into the disc space. A mixture of methylene blue and iopamidol is injected into the disc space for staining the disc (discogram). The needle is replaced by a guidewire and then a dilator is inserted into the disc space. This may cause some pain. Outer sheath is then inserted and dilator is removed. Endoscope is inserted and discectomy is done. If there are facetal osteophytes, they are removed by using burr, osteotomes, trephines, shavers, disc forceps. Once decompression is achieved, patient will experience relief from sciatica. Once adequate decompression is achieved, surgeon can visualized free floating dural sac. The instruments are removed and skin is closed with a single suture.
POST OPERATIVE CARE
Patient is shifted to the room once he is out of sedation. Patient can start normal diet one hour after the procedure. Patient can sit, stand and walk after the procedure. Patient is usually discharged from the hospital in a few hours. If the patient wants to stay overnight, he/she can stay overnight and can get discharged next day. Patient can have occasional pain in the lowerlimb or back for some time, up to two or three months. Generally, one stitch is used to close the wound. The dressing can be removed three days after the procedure and patient can have bath after that. Suture is removed 8 days after the procedure. Patient is advised one month of rest in general. Patient can sit, stand and walk depending on his pain tolerance. Patient can drive four wheelers after suture removal. Two wheelers are not good for the back and hence better avoided permanently. If the patient wants to use two wheelers, it can be done after a month, but not for long distance. Patient can resume normal duties after one month. The follow up is done at 1 month, 3 month, six months, one year and then yearly. We advice our patients to avoid lifting of heavy weights because this can cause recurrent disc prolapse. To have best results after endoscopic surgery, following advice should be followed.
- Avoid lifting of heavy weights.
- Reduction of weight if you are overweight or obese.
- Avoid prolonged sitting.
- Avoid long journeys.
- Stop smoking
- Avoid physical activity which you are not used to.
- Contact the doctor if you experience recurrence of pain.


- SPINAL CANAL STENOSIS: : Lumbar canal stenosis is a condition in which there is narrowing of the space in which the spinal nerves pass. It can be either central/ lateral or both. Patients with lateral canal (foraminal) stenosis do extremely well with endoscopic decompression.
- RECURRENT DISC PROLAPSE: Treatment of recurrent disc prolapse is a challenge even for an experienced spine surgeon. Recurrent disc prolapse can easily be treated with endoscopic discectomy. Patient does not require spinal fusion.
- DISCITIS: Discitis is a condition in which there is infection of the disc space. It is extremely painful and takes long time for recovery with traditional treatment. Sometimes, patient will end up with spinal fusion surgery. The causes may be iatrogenic (post operative), bacterial infection, tubercular infection. With transforaminal surgery, it is possible to debride, irrigate and decompress the infected disc. The disc material obtained is sent for biopsy and culture, the results of which will help in giving proper drugs to treat the infection. Transforaminal surgery helps the patient in rapid recovery, good pain relief, reduced hospital stay, reduced need for antibiotics and avoids fusion surgery.
- SPONDYLOLISTHESIS: Spondylolisthesis is a condition in which there is slippage of one vertebra over another. If there is nerve compression, it can cause sciatica or claudication. The definitive treatment for this condition is spinal stabilization and fusion which is a major surgery. If the patient wants a minimally invasive procedure for relief of leg pain, it is possible to do transforaminal decompression. However, patient should be ready for a second surgery/ spinal fusion at a later date.
- SPINAL BIOPSY:Spinal biopsy is indicated when there is suspicion of infection or tumor. It is possible to do endoscopic biopsy from the vertebra or the disc for diagnosis.
POST OPERATIVE CARE

Key hole disc surgery is a safe procedure in expert hands. The overall rate of serious complications in the literature is less than 1%. Infection, haematoma formation, nerve injury, dysesthesia, dural tears, bowel injury, vascular injury, instability, recurrence are some of the complications which may occur. The rate of infection is much less than open surgery because of minimum tissue trauma, continuous saline irrigation during surgery. Rarely patient can have transient post operative weakness of the lowerlimb due to stretching of the nerves. This temporary weakness of the lowerlimb recovers within a month. It is extremely rare to have permanent neurologic deficit as the patient is conscious during surgery and will not allow nerve damage to occur. Post operative numbness or dysesthesia is seen in few patients and may last up to three months. This usually responds to pregabalin and methylcobalamin capsules. If patient fails to respond to medical treatment, transforaminal steroid injection will help the patient. The complications such as bowel injury, vascular injury, instability, epidural fibrosis are extremely rare.
Recurrent disc prolapse: Recurrent disc prolapse is a common complication of any disc surgery, open or endoscopic. Recurrence can occur at the same level or other levels. The rate of recurrence is 2-12 percent after open discectomy. The rate of recurrence after endoscopic disc surgery is 3-6 percent. If there is recurrent disc prolapse, patient will experience recurrence of symptoms. It is diagnosed by clinical examination and MRI scan. If there is recurrence, it can easily be treated with keyhole disc surgery. Recurrence per se does not require fusion surgery.

